
What Are Autoimmune Rheumatic Diseases?
Autoimmune rheumatic diseases (ARDs) are conditions in which the body’s immune system mistakenly attacks healthy tissues, leading to inflammation and damage. They often affect the joints, skin, muscles, and sometimes major organs. This group includes Systemic Lupus Erythematosus (SLE or lupus), rheumatoid arthritis, scleroderma, myositis, Sjögren’s syndrome, amongst others. While the exact cause is not fully understood, most ARDs arise from a combination of genetic susceptibility, environmental triggers (e.g. infections, stress) environmental triggers (Environmental factors and rheumatic diseases, 2025), and hormonal influences – each playing a role in how the disease starts and progresses.
Why Are They Hard to Tell Apart?
Diagnosing ARDs can be challenging because these diseases often share similar symptoms and may even overlap. As the Global Autoimmune Institute (2022) highlights, some ARDs evolve into one another or occur together, and they often share similar blood test results. There are certain connective tissue diseases that have more specific features.
Why it’s complicated:
- Shared Symptoms: Fatigue, joint pain, swelling, and rashes are common across many conditions.
- Exclusive Features: Certain signs like the ‘butterfly rash’ in lupus, or thickened skin in scleroderma are more specific.
- Overlap Syndrome: Some patients meet the criteria for more than one ARD at the same time.
1. Rheumatoid Arthritis (RA)
Shared symptoms: Joint pain, joint stiffness (that improves with activity), swelling, fatigue.
Characteristic features: Persistent morning stiffness, symmetrical small joint involvement, risk of joint damage.
Rheumatoid arthritis is an autoimmune condition where the immune system mistakenly attacks the lining of the joints, often in the hands and feet. If untreated, it can cause progressive joint damage and disability. As well as joint pain, stiffness and swelling, symptoms may also include fatigue, low-grade fever, and inflammation in organs such as the lungs or eyes. Treatments, including disease-modifying anti-rheumatic drugs (DMARDs) and biologic therapy (Current perspectives on tocilizumab for the treatment of rheumatoid arthritis: a review), mean that with early diagnosis and regular specialist care, most people with RA manage their symptoms well and maintain active lives.
2. Systemic Lupus Erythematosus (Lupus)
Shared symptoms: Joint pain, rash, fatigue, low-grade fever.
Characteristic features: Butterfly-shaped rash over cheeks, kidney or lung involvement, recurrent mouth ulcers, and sun sensitivity.
Lupus is a complex autoimmune disease that can affect many parts of the body, including the skin, joints, kidneys, heart, and lungs. It is most common in women aged 15–44, with 90% of patients being female. Up to 30% of those patients with lupus, also have features of Sjögren’s syndrome. Because symptoms vary widely between individuals and over time, management takes a personalised approach; tailoring treatment to control inflammation, protect organs, and improve quality of life.
3. Sjögren’s Syndrome
Shared symptoms: Joint pain, fatigue.
Characteristic features: Dry eyes, dry mouth, dental problems.
Sjögren’s syndrome attacks the glands that produce tears and saliva, leading to the hallmark symptoms of persistent dryness, particularly of the eyes and mouth. Some patients also experience joint pain, rashes, significant fatigue, or small-vessel skin inflammation. It can occur alone, or alongside lupus or rheumatoid arthritis. Management focuses on easing dryness, preventing complications such as tooth decay, and controlling systemic inflammation.
4. Scleroderma (Systemic Sclerosis)
Shared symptoms: Joint discomfort, Raynaud’s phenomenon (a colour change most commonly in the digits, in response to cold or stress).
Characteristic features: Tight, shiny skin (especially fingers/face), swallowing difficulty, possible organ involvement
Scleroderma causes hardening and thickening of the skin, but it goes well beyond the surface, potentially affecting internal organs such as the lungs, heart, and digestive tract.
Because symptoms can vary widely, from mild to life-threatening, early diagnosis and personalised management, often tailored to controlling skin changes and slowing organ involvement, with a combination of medications and physical therapy, are key.
5. Myositis (Polymyositis / Dermatomyositis)
Shared symptoms: Fatigue, muscle aches, joint pain.
Characteristic features: Muscle weakness (hips, shoulders), muscle inflammation, distinctive rashes
Myositis refers to a group of rare autoimmune diseases characterised by muscle inflammation and progressive muscle weakness, especially in those muscles closest to the trunk (e.g. thighs and upper arms). Dermatomyositis (A case of anti-MDA5 dermatomyositis: the challenge of atypical skin manifestations) also produces characteristic rashes, for example, a violet rash on the eyelids (heliotrope rash) or scaly patches on the knuckles (Gottron’s papules). Muscle weakness may develop gradually, making everyday tasks, like climbing stairs or lifting objects, challenging. Treatment typically involves immunosuppressive medications, often with physiotherapy, to restore muscle strength and function.
6. Psoriatic Arthritis (PsA)
Shared symptoms: Joint pain, joint stiffness (that improves with activity), swelling, fatigue.
Characteristic features: Linked to psoriasis (skin/scalp plaques), nail changes, swollen ‘sausage-like’ fingers or toes (dactylitis).
Psoriatic arthritis is an inflammatory arthritis linked to psoriasis, a skin condition that can cause red or silver scaly patches. This arthritis can affect the joints, tendons, nails, and sometimes the spine. Because skin and joint symptoms may not appear at the same time, diagnosis can be delayed without specialist assessment; establishing the connection between skin and joint symptoms makes recognising PsA vital to preventing lasting joint damage. Treatment includes DMARDs and biologics to reduce inflammation and prevent joint damage.
7. Ankylosing Spondylitis (AS)
Shared symptoms: Joint pain, joint stiffness
Characteristic features: Inflammatory back pain and stiffness that improves with exercise, reduced spinal flexibility
Ankylosing spondylitis is an inflammatory arthritis primarily affecting the spine and sacroiliac joints. It often begins in young adults, and can cause long-term stiffness. Over time, the inflammation can lead to fusion of spinal bones, affecting posture and flexibility. Extensive research, including a summary in Nature Reviews Rheumatology (2021), highlights that while the exact cause of AS remains unknown, the disease uniquely combines autoinflammatory and autoimmune features. Early diagnosis and specialised care, including physical therapy, anti-inflammatories and biologic treatments, can help maintain flexibility and manage pain.
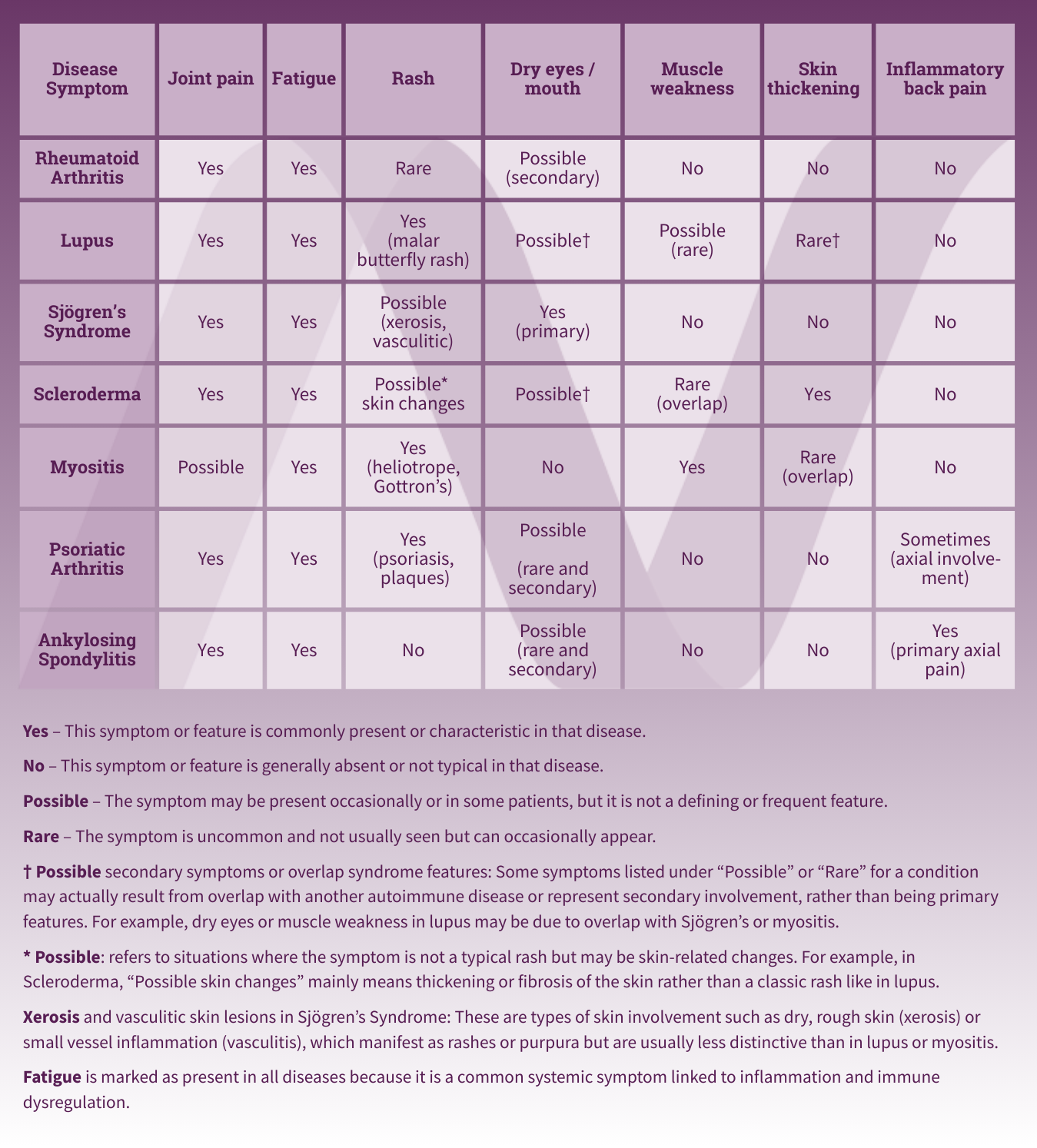
Table: Overlap of ARDs Symptoms
How Specialist Care Makes a Difference
ARDs are complex – they can mimic each other, evolve over time, or occur together. This means diagnosis requires specialist expertise in recognising subtle patterns, interpreting specialist blood tests, and using imaging or biopsies when needed.
“Getting the right diagnosis early allows for targeted treatment – significantly improving outcomes and preventing long-term damage.” Dr Israa Al-Shakarchi, MBBCh, FRCP (Rheum), MSc, BSc, PGCME, FHEA, Consultant Rheumatologist
The Diagnostic Process for ARDs
Detailed history – reviewing symptoms, flare patterns, and family history.
Physical examination – checking for specific rashes, joint swelling, Raynaud’s, muscle weakness or organ involvement
Blood tests – including ANA, autoantibody panels, ESR, CRP, and organ function tests
Urine tests – especially important for detecting lupus-related kidney disease.
Imaging/biopsy – to confirm diagnosis and assess internal organ involvement (e.g. X-rays, CT scan, echocardiogram, lung function tests, nerve conduction studies, electromyography)
FAQs
Q: Which autoimmune rheumatic disease is most common?
A: Rheumatoid arthritis is the most common, followed by lupus, Sjögren’s syndrome, scleroderma, and myositis.
Q: Can someone have more than one autoimmune rheumatic disease?
A: Yes. “Overlap syndromes” occur when patients meet the criteria for multiple conditions, highlighting the value of specialist care.
Q: How are these diseases diagnosed?
A: Rheumatologists use a mix of clinical examination, specialist blood tests (autoantibodies), imaging, and occasionally biopsies to reach a diagnosis.
Q: Why does diagnosis often take so long?
A: Because symptoms are non-specific and overlap, it often takes time and expert evaluation to pinpoint the correct disease. In rare diseases, diagnostic delays are not uncommon.
Take Action
If you have persistent joint pain, fatigue, or unexplained symptoms, it’s important to seek an assessment from a Consultant Rheumatologist. Early diagnosis and tailored treatment can dramatically improve quality of life and reduce the risk of long-term complications.
To book an appointment with our Consultant Rheumatologists, please call us on 020 8949 9020 or complete our online form:
Reviewed by Dr Israa Al-Shakarchi, Consultant Rheumatologist, New Victoria Hospital.












